The spine is a supportive structure in your body that starts from the skull base to the tailbone. It is the backbone and the central support structure of your body. The spinal cord, the main nerve track from the brain to the whole body, is present in the spinal canal surrounded by cerebrospinal fluid, which acts as a cushion and helps to protect the nerve roots and spinal cord from injury while performing activities, from sitting to bending and twisting.
As the name suggests, a degenerative spine disorder is often caused by our daily activities that cause stress and strain in the spine.
Depending on your activities and posture, movement and extent of stress and strain, the reaction of the spine – particularly vertebral bone, ligaments and joints – progressively lose their normal alignment, structure and, eventually, function.
Other than ageing, having tumours, infection, trauma, or arthritis will accelerate the degenerative process in the spine. Therefore degenerative spine disorders are not an uncommon problem in the elderly.
As you age, the consistency and flexibility of the spinal are reduced, making you vulnerable to developing degenerative spine disorders and subsequently limiting your movement and affecting your ability to practice your daily activities. Some common degenerative spine disorders are:
Cervical and lumbar spondylitis
Herniated disks or slipped disc with sciatica
Spinal stenosis
Facet joint arthritis etc
Classification of degenerative spine disorder depends upon the location of the affected spine (cervical, thoracic, lumbar, and sacrum).
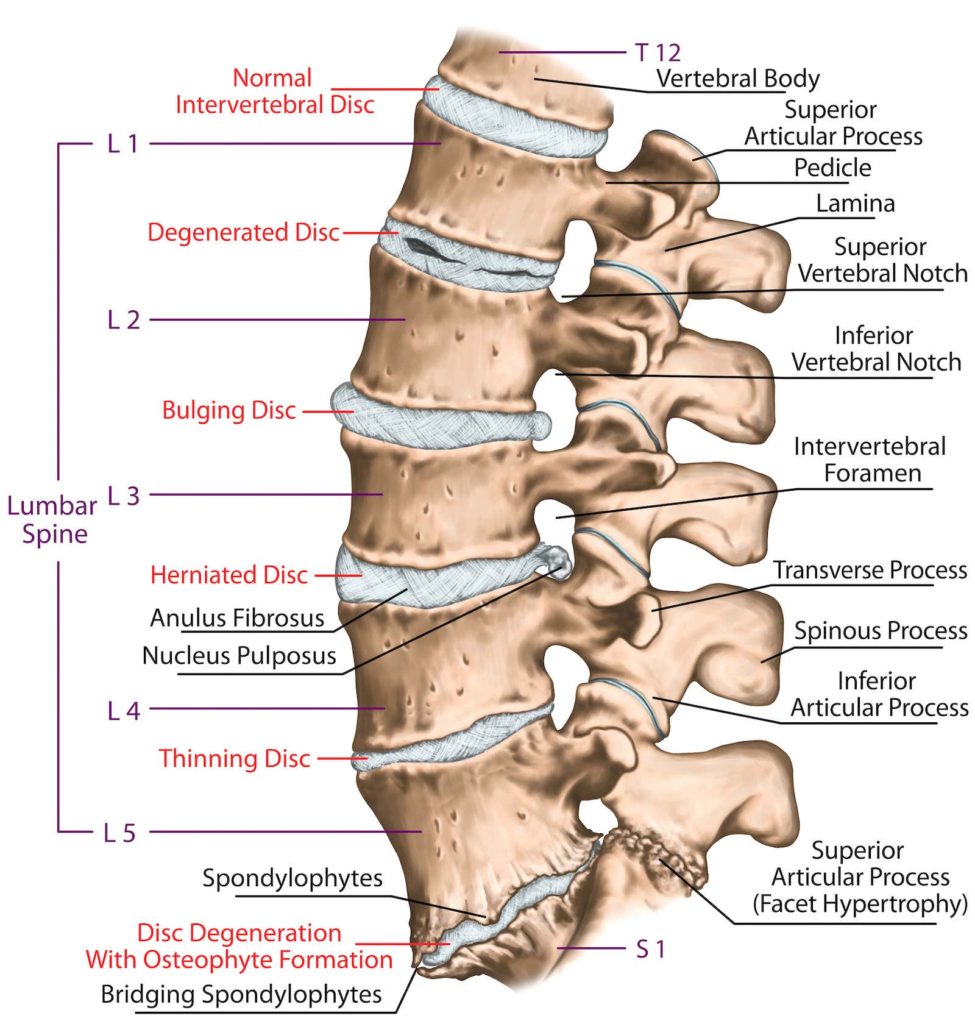
Spinal nerve root entrapment is the part and parcel of degenerative spine disorders. There are some reactive changes inside the spinal canal, as well as in the nerve root openings that pinch or press the spinal cord and nerve roots.
The initial part for irritation and compression cause severe nerve root pain and significant muscle spasms in the affected nerve root areas. Subsequently, patients may feel numbness if the compression is severe enough to damage the nerve or spinal cord. It most commonly involves:
It is a condition where the lumbar nerve gets compressed in the lower back of the spine and is characterised by severe lower back pain radiating towards the leg. It is most frequently caused by a herniated disc or bone spurs at the nerve root openings or slipping of vertebral bone during long periods of standing or sitting postures.
This condition is caused by a compression in the cervical part of the neckbone. Patients generally experience severe pain in the neck radiating towards the arm, shoulders, and upper portion of the back (the area in between the two shoulder blades).
Some of my patients complain of very unpleasant feelings and not knowing how to position their heads at night, finding it difficult to sleep.
The mechanism of spinal instability is somewhat unclear as the spine is a mobile axial bone in our body. During its movement, either bending or twisting, the stability of the spine depends on the quality of vertebral bones in the spine together with the disc between the bodies of the vertebra, as well as the muscle bulk behind the spine, the facet joints behind the vertebral body and ligaments that attach to the spinous processes. They are the main supporting elements in the spine.
Any injury or disease affecting these elements can progress to the instability of the spine, which may eventually lead to compression of either the spinal nerve roots or spinal cord at the affected level. Therefore, spinal instability is associated with a spinal injury (muscular) and degenerative changes (age-related changes). These progressive changes can be triggered by:
Cervical spine disorders most commonly present with neck and shoulder aches, and subsequently, arm pain and numbness or electric shock-like sensations in the arms and fingers. They are most commonly caused by ageing, trauma (whiplash injury), and daily stress and strain from abnormal head and neck postures.
Nowadays, abnormal head and neck postures with early degenerative changes in the cervical spine are very common among those in younger age groups, people who excessively use their smartphones, employees with deskbound jobs and highway or taxi drivers who drive for long periods.
The cervical spine associated with disc herniation or spinal cord compression is the most severe condition that requires prompt decompression and appropriate treatment. It may result in severe nerve root or spinal cord damage, resulting in total paralysis and permanent disability if left untreated. Cervical spine disorders are:
A lumbar prolapsed disc is caused by the rupture of the outer fibrous membrane of the spinal disc which causes the protrusion of inner soft gelatinous material called nucleus pulposus. The extruded disc material presses or irritates the surrounding nerve roots, causing inflammation and stimulation along the nerve fibres.
It is characterised by severe back and radicular pain in the legs associated with numbness and paraesthesia. It restricts the movement of the affected limb due to pain and subsequently, it can worsen to paralysis of the affected nerve (similar to limping gait in patients with stroke).
Symptoms of these spine disorders depend on the structure and portion of the spine involved.
Degenerative spine disorders are high-risk disorders. If left untreated, they can lead to paralysis of the affected limb. Set an appointment with your neurosurgeon whenever you have the following symptoms.
Prompt treatment is required after diagnosis.
Multiple factors are involved in causing degenerative spine disorders. Such as:
● Ageing
● Trauma
● Sport injury
● Inflammation (arthritis)
● Scoliosis (abnormal spine alignment: either congenital or degenerative)
● Infection
● Tumours (primary or secondary)
● Inactivity (bed bound/wheelchair-bound due to stroke/ trauma)
● Congenital or acquired neuromuscular disorders (multiple sclerosis)
● Endocrine disorders affecting bone
● congenital/ genetic disorder affecting axial spine (ankylosis spondylitis)
● Smoking
● Obesity
An important part of the diagnostic process involves getting a detailed history of your symptoms, lifestyle, and personal and family history. After which, I would conduct a general physical exam, neurologic assessments and other diagnostic tests.
In order to accurately diagnose your disorder, certain tests are run, such as:
A powerful magnetic field and radio waves are used to provide a clearer image of the affected site and the nerves involved.
A CT scan is used to better visualise the vertebrae (bones of the spine) and other spinal structures and tissues to provide more information on the spine’s structure and spinal tissue.
Full-body 3D images of the spine to examine its alignment. These images are created with the patient in a natural, standing position. An EOS scan emits much less radiation compared to CT scans and x-rays.
Low dose x-rays are used to measure bone density and the mineral content of the bones.
Dynamic x-ray shows a structural instability of the spine during movement of the spine.
Urodynamic studies are a series of tests that help assess the bladder and its sphincter function related to the spinal cord and nerve roots.
This helps diagnose nerve roots and peripheral nerves together with their supplied muscle groups by measuring the electrical activity and sensitivity of the muscles and nerves.
Treatment of degenerative spine disorders depends upon the type and severity of the disease, severity of nerve roots involvement and stability of the spine.
Basically, not all degenerative spine disorders require surgical intervention. Proper assessment and evaluation are the main steps for the initiation of treatment. Options of treatments are:
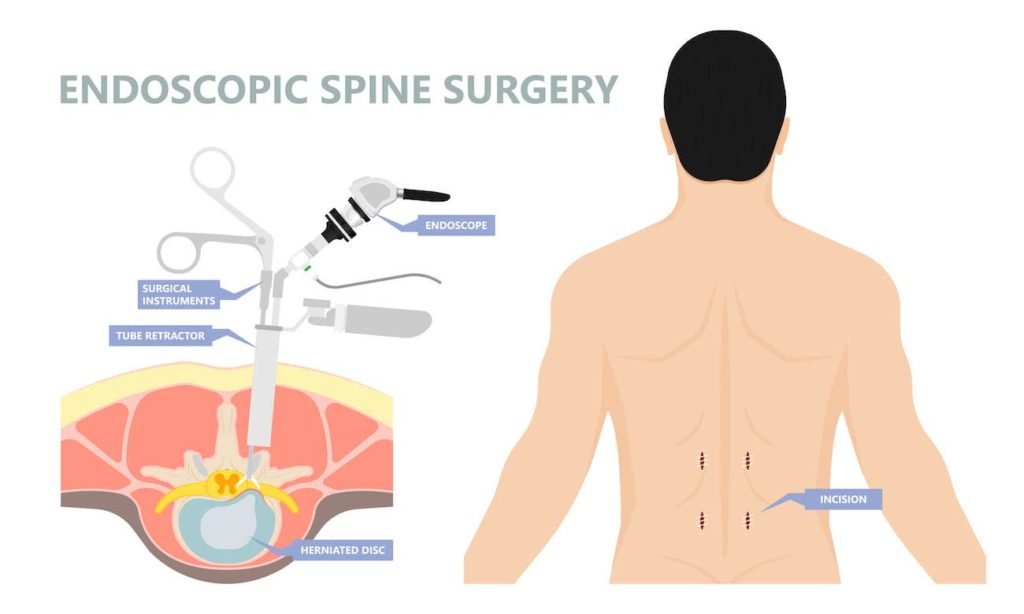
A discectomy is carried out to remove the herniated disc to relieve the pressure on the nerve root or spinal cord. Often, it is carried out via a minimally invasive approach, called an MIS microdiscectomy, where small incisions with a narrow space are made under a microscope or endoscope and the disc causing pressure over the nerve or spinal are removed.
It is a very short procedure with less damage to the surrounding tissues with minimal pain at the operative site. The patient can ambulate immediately after the procedure and may go home on the day of the surgery or stay in the hospital overnight.
This is a surgical procedure that creates more space for the nerve roots at their exits or spinal cord. This procedure helps relieve pressure caused by the thick ligaments or bony spurs due to degenerative changes in the spine.
Decompression alone can help to lower spinal canal pressure in the spinal cord and improve spinal blood supply, relieving inflammation and congestion in the spinal cord. This, in turn, relieves pain in the lower area of the spine and along the nerve roots in the legs.
This is a post-decompression surgical procedure in which specific metal implants (screws or rods with artificial discs) are inserted to reinforce the stability of the affected spinal area. Stability of the spine is important for the spine’s alignment and subsequent early mobilisation of patients after surgery.
Degenerative spinal nerve disorders are the most common age-related condition associated with nerve pain and numbness in the affected areas. These are related to loss of spinal alignment which causes further damage to the nerve roots and spinal cords when handling heavy objects, walking, bending, and twisting.
Spinal nerve disorders should be diagnosed and treated as early as possible because they can lead to permanent damage and paralysis of the affected limb.

Senior Consultant
Neuro & Spine Surgeon
MBBS, MSc Surgery, MRCS (Edin),
MMed. Sc (Gen Surg) (S'pore),
FRCS. Surgical Neurology (UK)
Dr Sein Lwin is an experienced Senior Consultant Neuro & Spine Surgeon and the Neurosurgical Director at the Advanced Brain and Spine Surgical Centre.
He is highly experienced in spine surgery and in minimally invasive approaches for spinal cord tumours and degenerative spine surgery. His specialised interests lie in endoscopic endonasal and open skull base surgery, pituitary tumours, vascular surgery, cranial nerve disorders and peripheral nerve conditions.
Many neurological conditions may require urgent attention. If you require immediate care, please contact us.
Contact Us For More Information
Your needs are important to us.
For enquiries, leave a message and our friendly team will get in touch with you.
Monday – Friday: 9:00AM – 5:00PM
Saturday: 9:00AM – 12:30PM
Sunday & Public Holiday: Closed
We provide quality specialised care for neuro and spine conditions.
For enquiries, leave a message and our friendly team will get in touch with you.
Monday – Friday: 9:00AM – 5:00PM
Saturday: 9:00AM – 12:30PM
Sunday & Public Holiday: Closed
We provide quality specialised care for neuro and spine conditions.
For enquiries, leave a message and our friendly team will get in
touch with you.
Monday – Friday: 9AM – 1PM | 2PM – 5PM
Weekends & Public Holidays: CLOSED
© 2023 All Rights Reserved | Advanced Brain & Spine Surgical Centre | Terms & Conditions